Plantar Plate, pearls and pitfalls

Plantar Plate, Pearls and Pitfalls
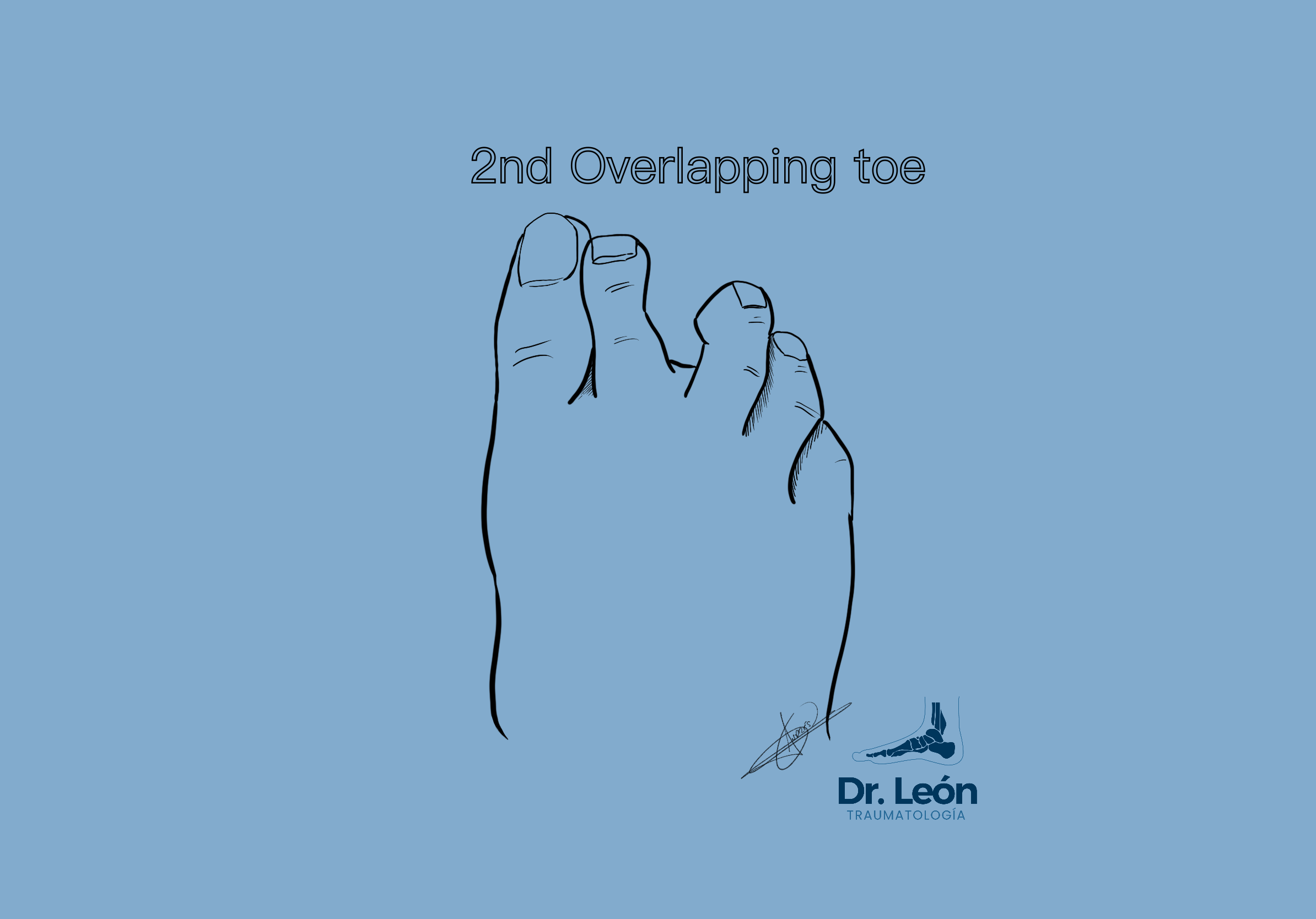
Coughlin in 1987 described the crossover toe by seeing an overlapping of the second and first toes. However there is an increasing awareness and interest in diagnosing and treating these deformities in their early stages.
V Sign
V Sign related to second space syndrom and Crossover toe related to Hallux Valgus and PP injury
How does Morton neuroma, metatarsalgia, overlapping toe, floating toe, second space syndrome relate to the plantar plate?
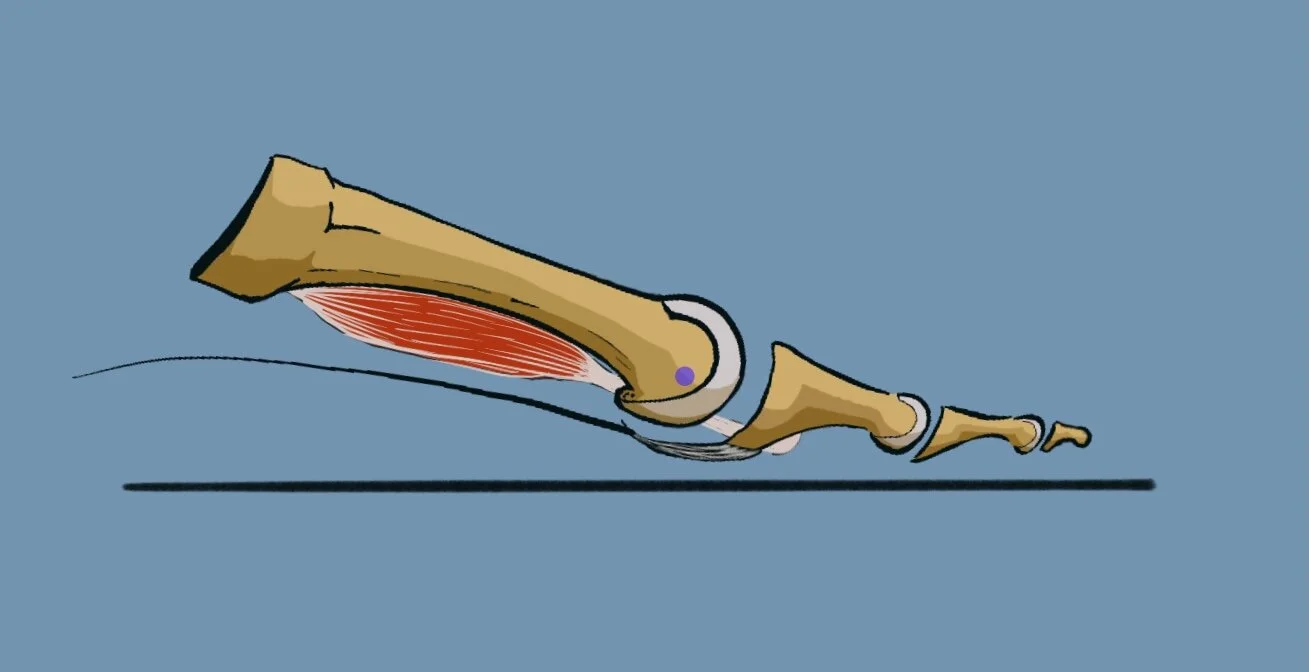
The Plantar Plate (PP) is a fibrocartilage structure plantar to the metacarpo phalangeal joint (MTPJ), it works as a restraint of the dorsiflexion of the toes. It is responsible for cushioning and offloading compressive forces, being part of the windlass mechanism. The PP structure is primarly made from fibrocartilage and collagen type 1. It has also deficient vascularization in the middle 1/3rd.
Plantar plate anatomy, ligaments and plantar fascia
First of all, not all PP injuries evolve to a crossover toe. MTP joint instability does not necessarily deviate medially in every case.
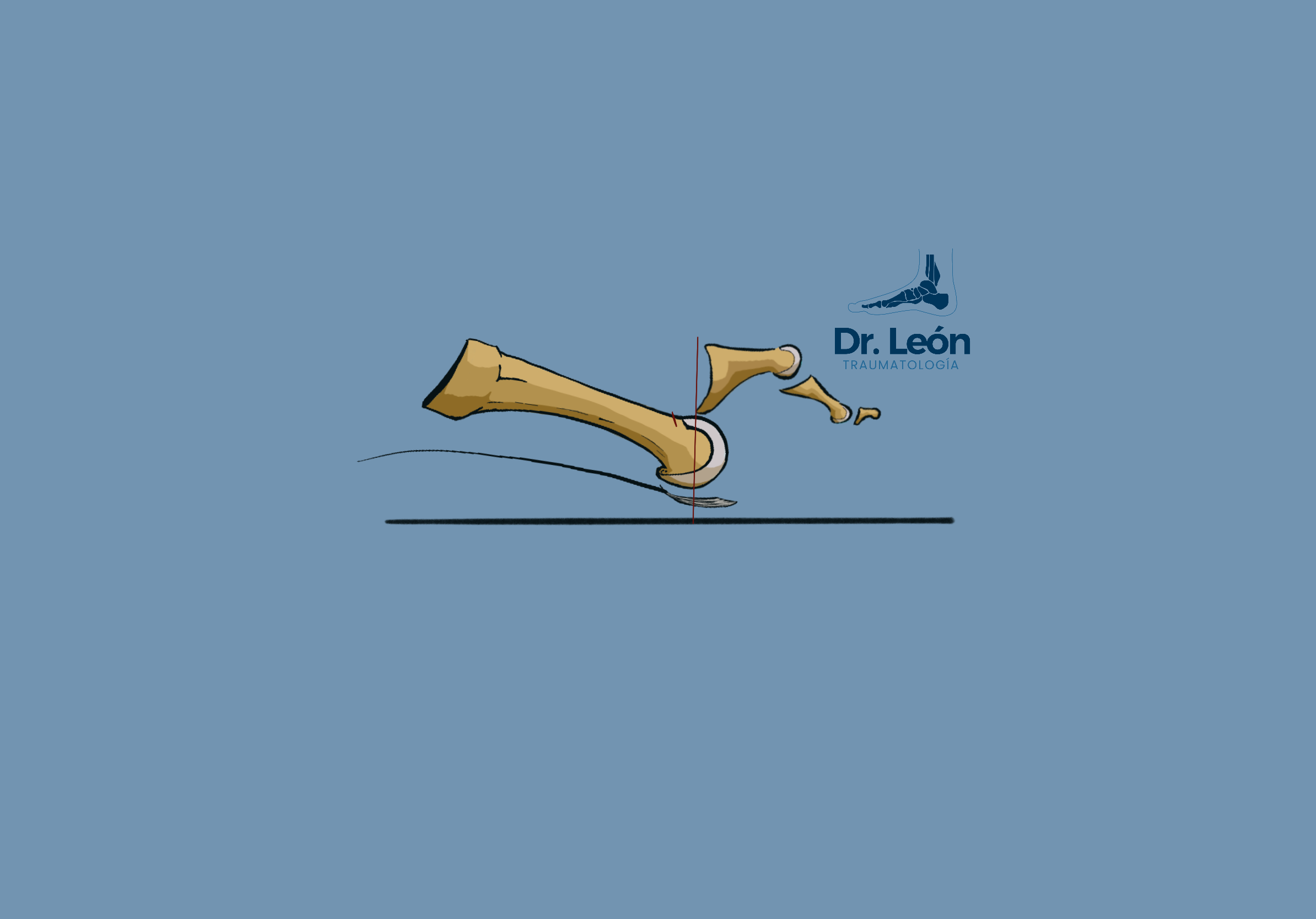
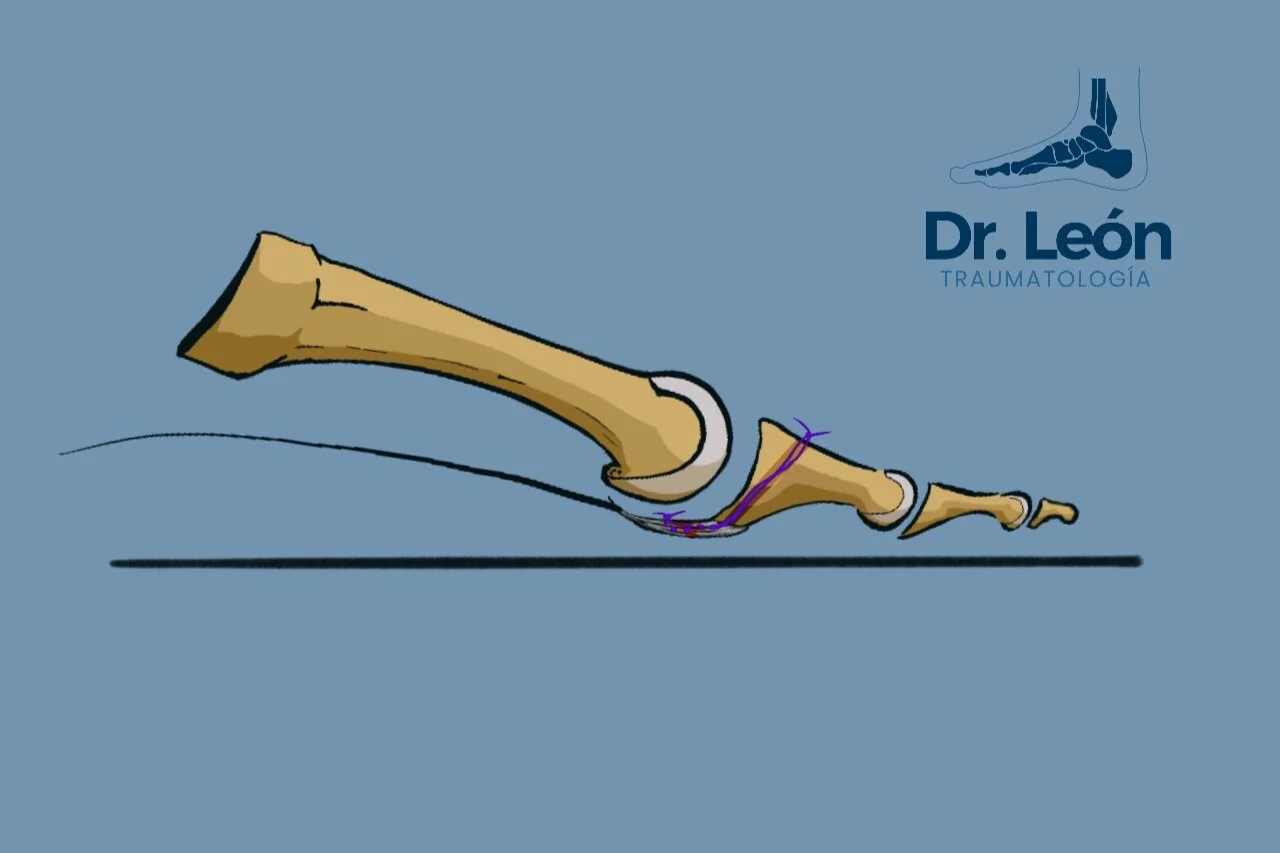
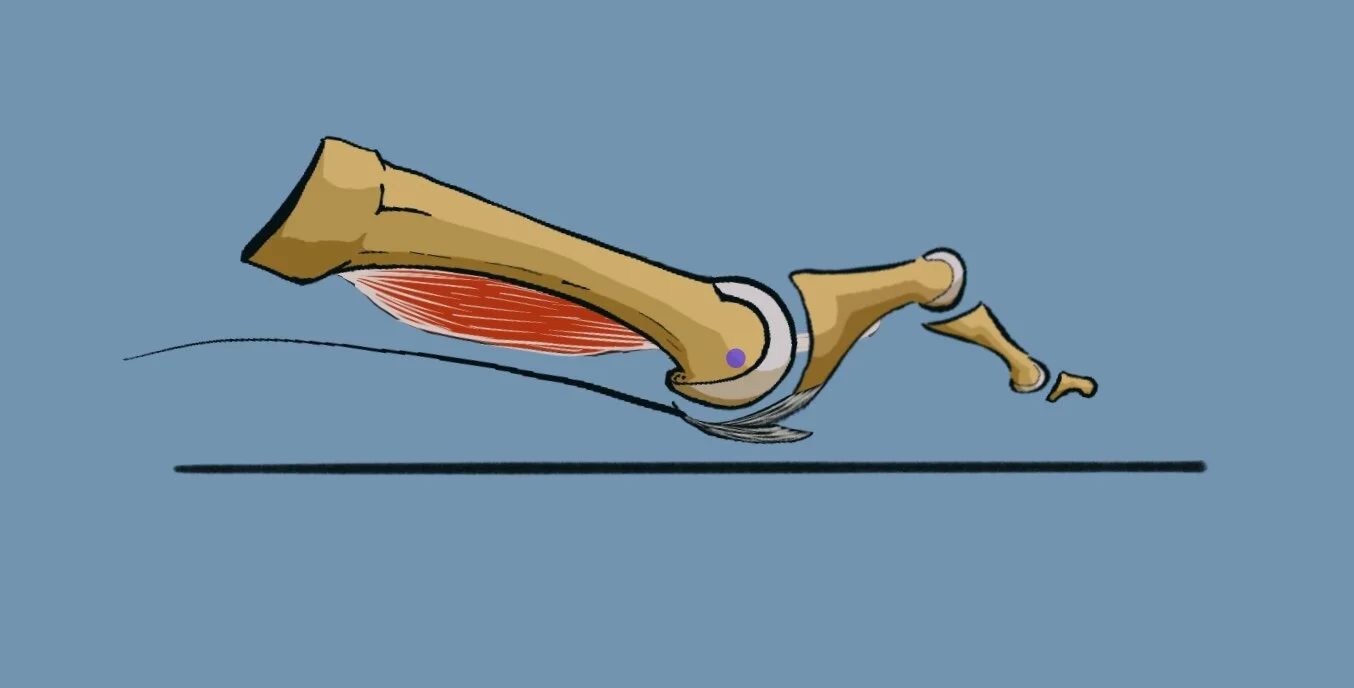
However classic presentation begins with floating toe, varus deviation of the 2nd toe (more frequently), divergence of the 2nd and 3rd toes. Deformity is amplified by loosening of the intrinsic muscles as a plantar flexion force in the early stages of dorsal dislocation and in third rocker, when the pull vector goes above the center of rotation of the MTP joint and becomes a force of extension.
Losing the PP cushioning leads to third rocker metatarsalgia. Dorsal subluxation first leads to hammer toe deformity and then to floating toe as the deformity progresses. Chronic ruptures and deformity becomes fixed deformities.
There needs to be a differential diagnosis between Interdigital neuroma and plantar plate lesion. There are too many patients that are mis-diagnosed with “Morton’s neuroma of the second space” while receiving treatment for a pathology that doesn’t cause them pain.
Why does the Plantar plate ruptures?
During the third rocker, the forefoot experiences 120% of body load. Increasing the risk of PP shear injuries. PP is also a checkrein to dorsal displacement of the toes in the MTP.
Most common cause is chronic attritional wear in the midportion of the PP due to microvasculature deficiency.

Plantar plate attrition lession
What to look for in patients that Plantar plate rupture is suspected?
Pain at the MTP joint, most common in the 2ºnd toe
Third rocker metatarsalgia
MTP paper test (klein et all)
DRAWER TEST - Thompson and hamilton 1987
V sign
Crossover toe. Late stages
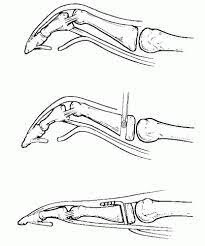
Drawer Test
With one hand stabilize the metatarsal, while with the other hand pinch the base of the Proximal phalanx.
Trying to subluxate the Phalanx dorsally is how to properly apply this test.
In early stages pain but no movement is common, in late stages the phalanx is dorsally dislocated
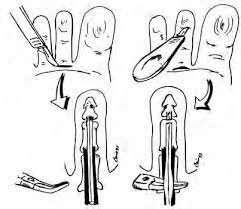
Plantar Plate Test
Test is positive - Pathologic (PP injury suspected)
when there is no purchase between the toe and the flor
The piece of paper slips easily
Test is negative
when there is a break of the piece of paper as the purchase of the toe to the floor is strong enough to not be overcome.
TEST are NOT VALIDATED
Nery has published his results of looking into MTP joints of hundreds of patients.
However the results show that there are more G3-G4 lesions than G0-1-2
Meaning that there are lots of patients with PP injured that are probably being infradiagnosed
Do I order some more test?
PP injury is mostly a clinical entity, however having a weight bearing xray of the foot is critical to many diagnoses. For the PP the signs appear late in time

MRI is the best test, with results ranging from 96% sensibility and 95% specificity. However, prices and waiting lists may not be worth it.
Ultrasound as always is operator dependent and it has sens/specif lower than MRI. Some say to check with US and some say not to (klein)
For me physical exploration and Xrays are the only test needed.
Do we always need to repair the PP and when?
Some authors, centered around the biomechanics of the foot, defend that PP injury is produced in most cases by a mechanical overload under the metatarsal head. Biomechanically restoring the anatomy by means of osteotomies can offload the PP and let it heal. There is evidence relating improvements of the symptoms when the anatomy is restored, however there are toes that deform again and not all cases can be attributed to the most common risk factors.
PP direct repair
Using mattress sutures to fix the PP to the Proxima phalax.
(Click the image to go to Youtube)
Risk factors
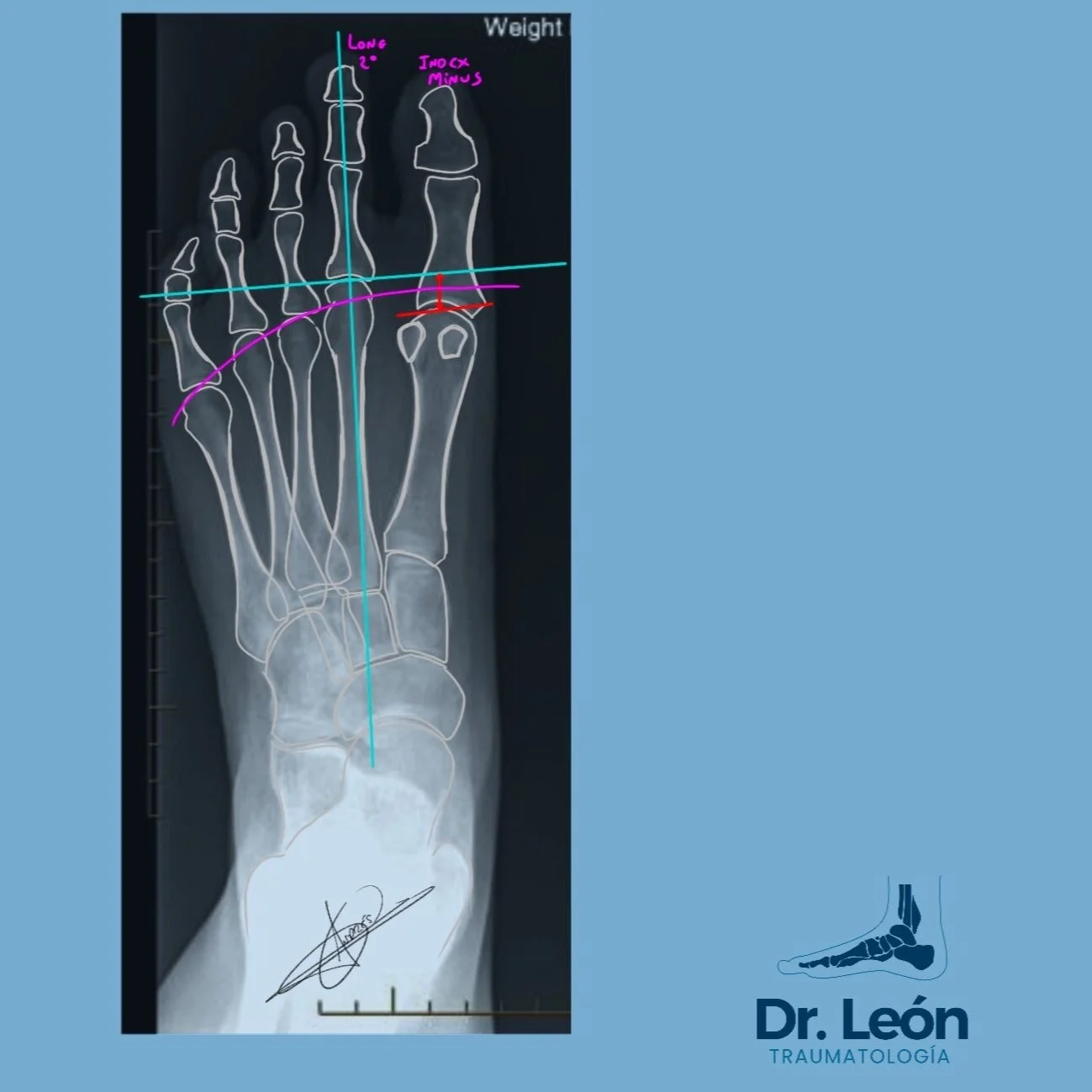
Index minus + long 2nd metatarsal - At risk of PP injury
First ray pathology - Index Minus
Second ray longer (Chronic attritional wear)
Shoe wear
Trauma (acute Rupture)
Inflammatory arthropathy (synovitis)
There is also an association with HR and HV
Even if there are not many paper reviewing how and by how much does the suture help with the healing of the PP there are promising results following direct repairs.
Real life Constraints
Time to surgery, at least in Spain, is a very lengthy process. Even up to 2 years of waiting list. That is why even early PP diagnosis can worsen until surgery.
Concomitant foot procedures to PPR have been shown to be related to more complications (Stiffness and loss of movement)
PP diagnosis is challenging
Subtle clinic
delay in diagnosis
How can we treat PP injuries?
Early stages treatment
Well fitting shoe to reduce overload
Metatarsal pads and extra depth shoes - to alleviate discomfort
Injections?? not enough evidence - Thought to be a risk to rupture plantar plate. not rutinely done
Surgery is indicated to restore toe elevation and angular defformity
Dorsal approach more used, plantar is more direct but need careful dissention of the NV bundle and increased risk of fibrosis.
There are countless techniques to treat PP injuries. Some are as follows
Sinovectomy
Capsulotomy
Extensor tendon lengthening
Bony decompresion (weil and triple weil osteotomy)
PP repair
Whatson - mini scorpion and fiberwiker mattress repair + drilling in base of PF
FT transfer
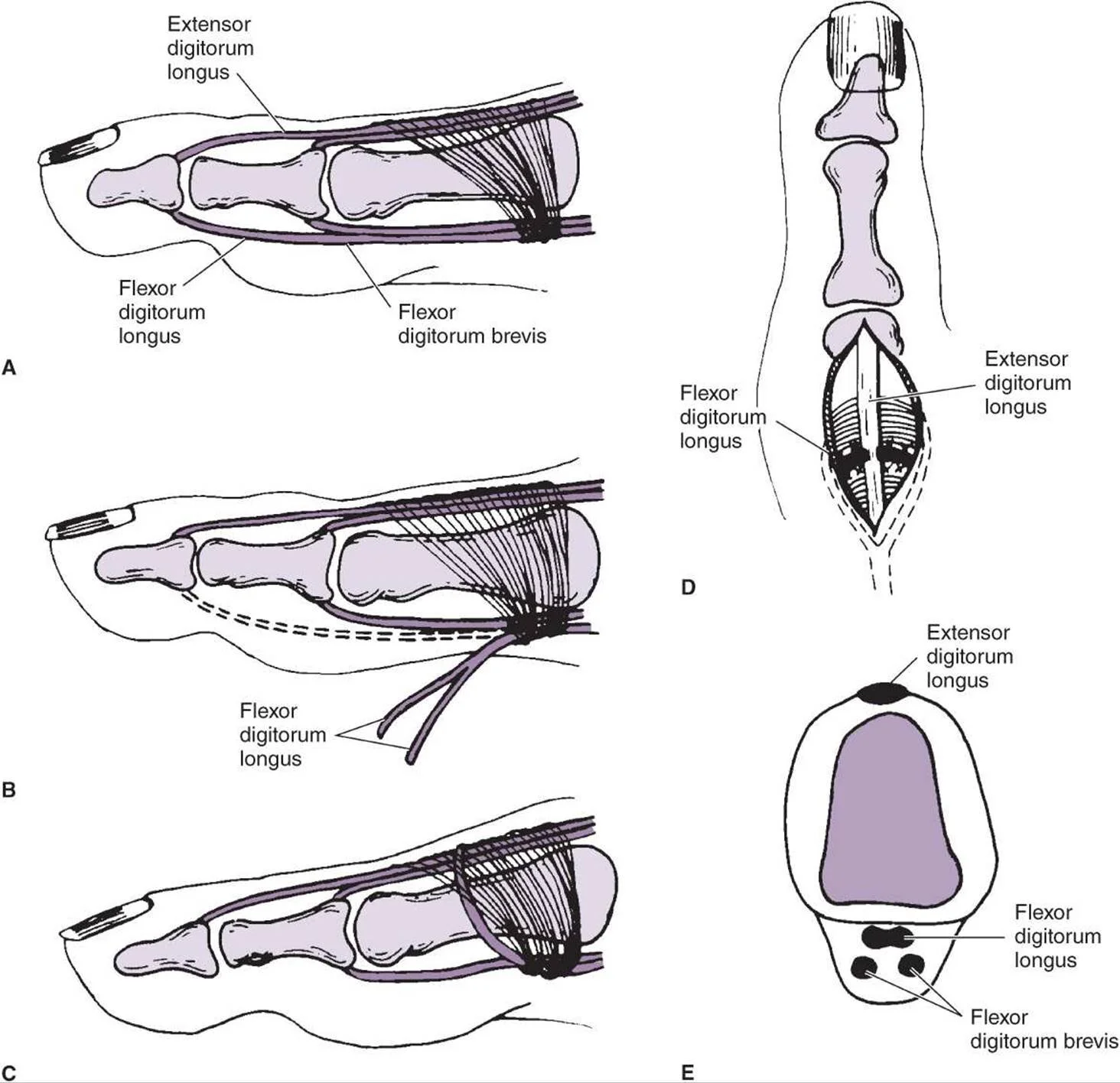
Girdlestone-Taylor flexor to extensor tendon transfer, associated with weil osteotomy when the phalanx is completely dislocated or as an isolated technique in other pathologies (Flexible hammer toe)
Nery recommends
Grade 0-1 synovectomy - arthroscopy
2-3 weil and direct repair
4 grade -> need flexor tendon transfer to extensor tendon
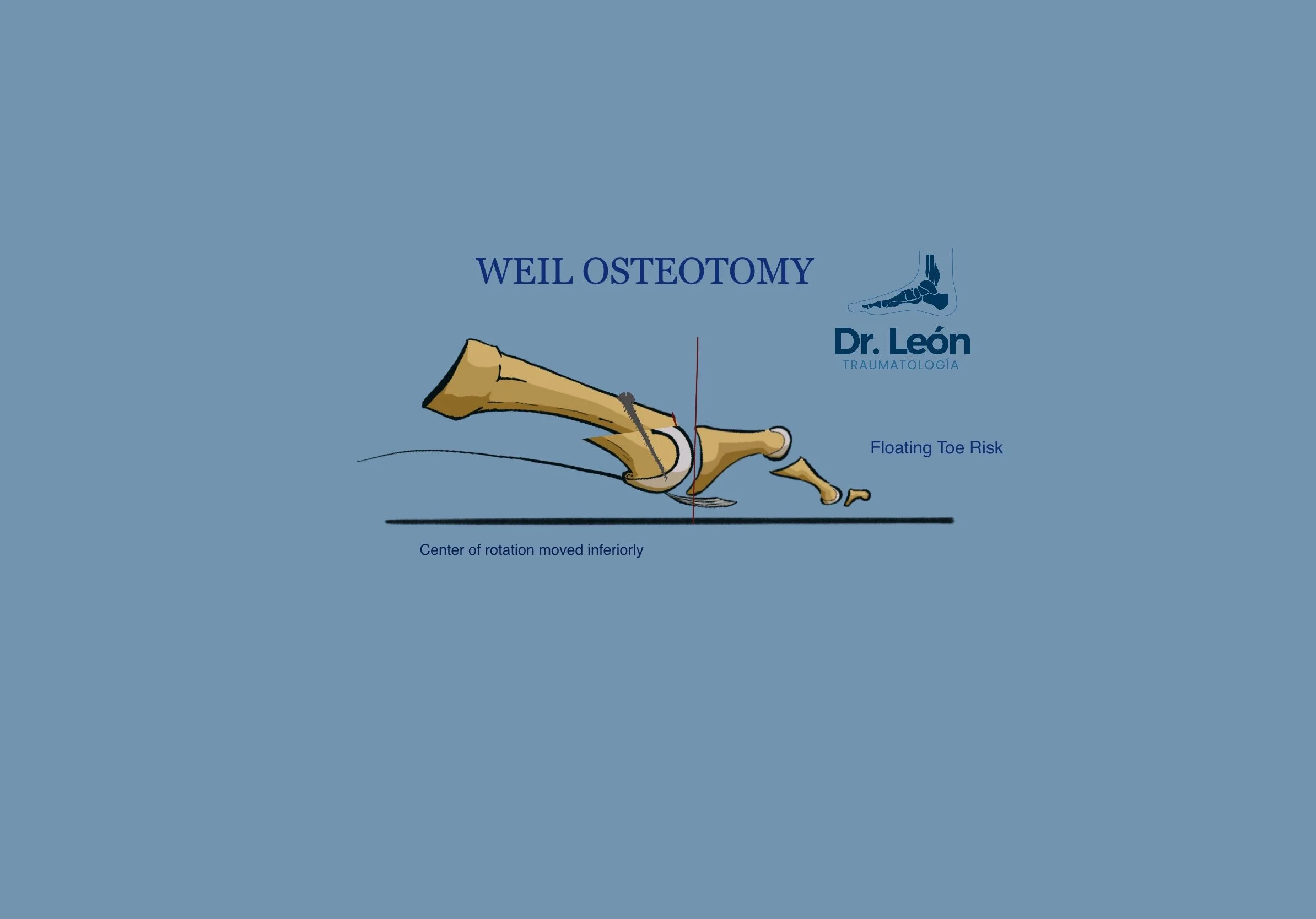
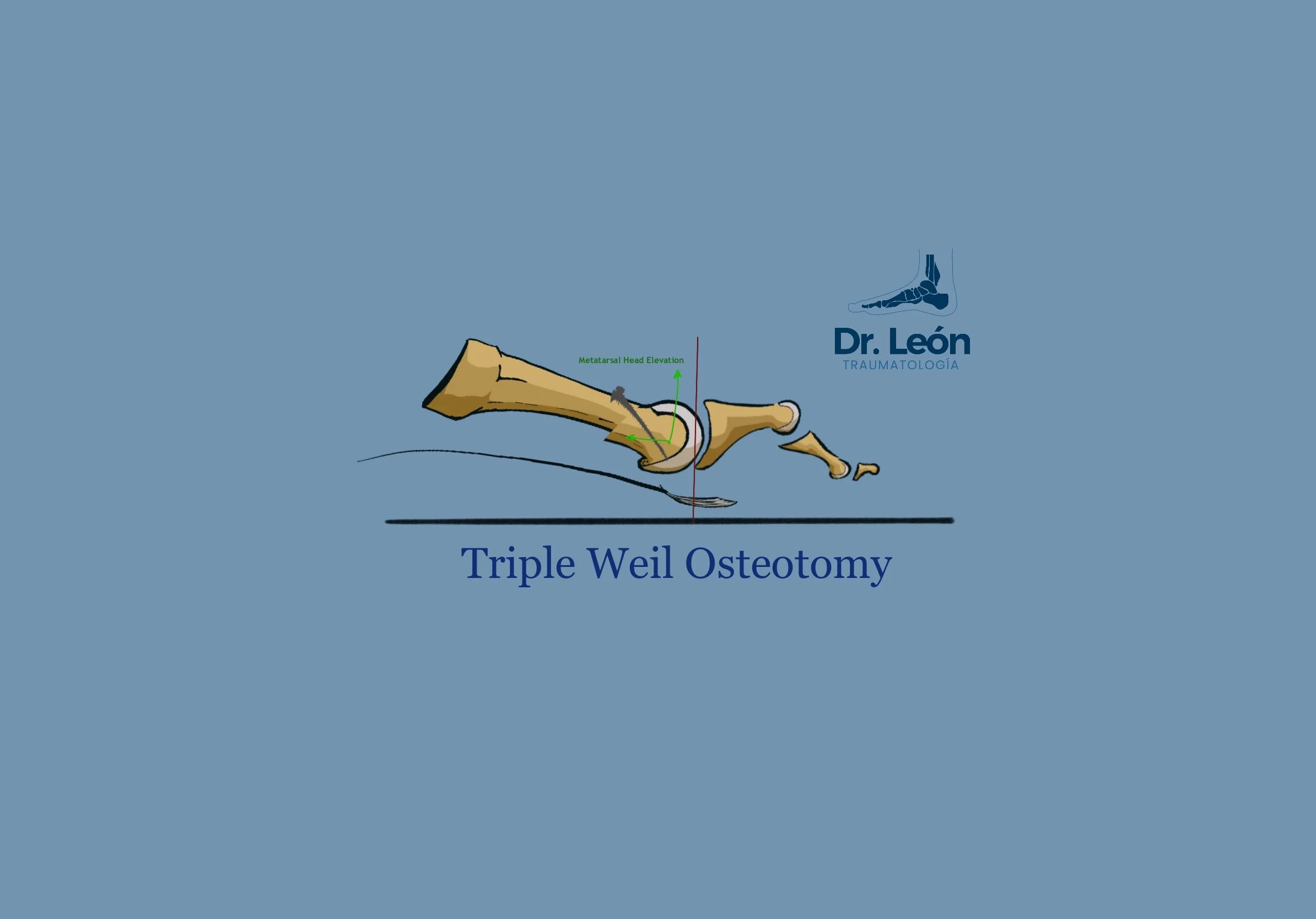
Simple weil vs Triple weil Osteotomy?
Simple weil osteotomy shortens the metatarsal length to restore Maestro’s line
(relationship between metatarsal heads) However it is associated with second rocker metatarsalgia and floating toes(36%) and recurrence of the symptoms (15%). There is also rigidity associated with the dorsal approach and fibrosis related to the scar.
Triple weil osteotomy (Maceira’s osteotomy) is a three cut process that elevates the head of the Mtt while shortening it. It maintains the center of rotation elevated leading to a decrease in the rate of second rocker metatarsalgia and floating toes.
After surgery, What should I tell my patients?
There is some evidence favouring active + passive plantarflexion of the toes as pain permits. Also limiting dorsiflexion of the toes with the dressing prevents new ruptures in the healing plantar tissues.
Caio nery recomends:
aggressive active and passive plantar flexion of toes
Limit or prohibit dorsiflexion of toes
Bandage of toes in plantar flex position 20º
Walk protected for 6 w then 3 months of wide or MBT shoe
One of the more frequent complications after surgery is to have a floating toe.
The floating toe is one that has lost the ability to press on the floor efficiently, there are not many times that this deformity is functionally relevant, but there is one of the leading complaints of patients and surgeons following weil osteotomy.


Causes of Floating toes following Weil osteotomies
Depression of the mtt head (alterating center of rotation)
Loss of tension in PP
Mtt shortening
How to decrease Floating toes?
Myerson and jung, 64 feet . por results from flexor tendon transfer - only 39% toe contact
Doing weil + PP repairs
Floating toes goes from 33% to 18%
Take Home Message
Confusing evidence -> Too many associated procedures and heterogenous group.
Many techniques -> not so stellar results.
Two ways of thinking
Repair the soft tissue.
Restore bone anatomy and biomechanics.
Probably there is a combination of both procedures that gives the best results.
Challenging diagnosis, at least in the early stages.
Close follow up of this patients is imperative after surgery to minimise wound complications, teach rehab and maintain correctly positioned dressings.
Always take some wight bearing xRays.
Bibliography
Akoh CC, Phisitkul P. Plantar Plate Injury and Angular Toe Deformity. Foot Ankle Clin. 2018 Dec;23(4):703-713. doi: 10.1016/j.fcl.2018.07.010. Epub 2018 Sep 25. PMID: 30414662.
Elmajee M, Shen Z, A'Court J, Pillai A. A Systematic Review of Plantar Plate Repair in the Management of Lesser Metatarsophalangeal Joint Instability. J Foot Ankle Surg. 2017 Nov-Dec;56(6):1244-1248. doi: 10.1053/j.jfas.2017.05.039. Epub 2017 Sep 8. PMID: 28893531.
Nery C, Umans H, Baumfeld D. Etiology, Clinical Assessment, and Surgical Repair of Plantar Plate Tears. Semin Musculoskelet Radiol. 2016 Apr;20(2):205-13. doi: 10.1055/s-0036-1581114. Epub 2016 Jun 23. PMID: 27336454.
Linklater JM, Bird SJ. Imaging of Lesser Metatarsophalangeal Joint Plantar Plate Degeneration, Tear, and Repair. Semin Musculoskelet Radiol. 2016 Apr;20(2):192-204. doi: 10.1055/s-0036-1581115. Epub 2016 Jun 23. PMID: 27336453.
Besse JL. Metatarsalgia. Orthop Traumatol Surg Res. 2017 Feb;103(1S):S29-S39. doi: 10.1016/j.otsr.2016.06.020. Epub 2017 Jan 18. PMID: 28109624.
Prissel MA, Hyer CF, Donovan JK, Quisno AL. Plantar Plate Repair Using a Direct Plantar Approach: An Outcomes Analysis. J Foot Ankle Surg. 2017 May-Jun;56(3):434-439. doi: 10.1053/j.jfas.2016.12.002. Epub 2017 Jan 27. PMID: 28139400.
Finney FT, McPheters A, Singer NV, Scott JC, Jepsen KJ, Holmes JR, Talusan PG. Microvasculature of the Plantar Plate Using Nano-Computed Tomography. Foot Ankle Int. 2019 Apr;40(4):457-464. doi: 10.1177/1071100718816292. Epub 2018 Dec 19. PMID: 30565497; PMCID: PMC6443423.
Flint WW, Macias DM, Jastifer JR, Doty JF, Hirose CB, Coughlin MJ. Plantar Plate Repair for Lesser Metatarsophalangeal Joint Instability. Foot Ankle Int. 2017 Mar;38(3):234-242. doi: 10.1177/1071100716679110. Epub 2016 Nov 16. PMID: 27852647.
Case series plantar plate repair + weil - 1 year (dorsal approach)
138 tears in 97 feet
Vas, aofas, rom, pull out test, xray, satisfaction
improvement in vas, aofas
42% paper pullout test -> 54% at the end (Strength)
More floating toe
Reduced joint motion expected if PPR +
Clements JR, Ghai AK. An Innovative Method for Plantar Plate Repair: Technique Guide and Case Report. J Foot Ankle Surg. 2019 May;58(3):555-561. doi: 10.1053/j.jfas.2018.09.006. Epub 2019 Mar 20. PMID: 30902492.
Klein EE, Weil L Jr, Weil LS Sr, Coughlin MJ, Knight J. Clinical examination of plantar plate abnormality: a diagnostic perspective. Foot Ankle Int. 2013 Jun;34(6):800-4. doi: 10.1177/1071100712471825. Epub 2013 Jan 14. PMID: 23696184.
Nery C, Coughlin MJ, Baumfeld D, Mann TS. Lesser metatarsophalangeal joint instability: prospective evaluation and repair of plantar plate and capsular insufficiency. Foot Ankle Int. 2012 Apr;33(4):301-11. doi: 10.3113/FAI.2012.0301. PMID: 22735202.
Coughlin MJ, Baumfeld DS, Nery C. Second MTP joint instability: grading of the deformity and description of surgical repair of capsular insufficiency. Phys Sportsmed. 2011 Sep;39(3):132-41. doi: 10.3810/psm.2011.09.1929. PMID: 22030949.
Most of the Images in this Blog are made by me with Procreate 5 for the Ipad (newby artist). The rest are taken from the Google Images. Last Edit or update of this Post: 20/07/211
If what you have read it’s of your liking take a look at other post and follow on social media for new content and updates in orthopaedic surgery.