Infiltrating the Plantar Fascia
Free Link to google document -> Best source to save and free Questions to test your knowledge
Is it effective to Infiltrate the Plantar Fascia?
For years one of the Gold Standards for the treatment in plantar fascitis has been infiltrating it with corticosteroids. Recent publications shed more light on the matter. Updating our knowledge may be beneficial to give our patients the best care we can with the available evidence.
Kamonseki compared stretching exercises and strengthening of the foot and hip and found improvement post 6 months in every group
Johannsen in 2019 studied the associations between injections and exercises. It concluded that the combination of treatments gave the best results. That is why the first line of treatment is corticosteroids injection associated with strength and stretching programs. This combined treatment is superior both in the short and in the long term to doing just one or the other. (Example of stretching and strengthening program)
Second line treatments include Shock wave therapy at 6 months of non effective treatment. And surgery is relegated to third line 9-12 months of failure of other treatments (Proximal Medial Gastrocnemius recession, ⅔ medial proximal plantar fascia release or Tarsal tunnel decompression)
It is important to do a differential diagnosis between plantar fasciitis and Baxter neuropathy or other nerve compression syndromes of the foot (Plantar nerves or posterior tarsal tunnel). There has been new interest recently in the association between plantar fasciitis, tibial posterior tendon insufficiency (pes planus) and posterior tarsal tunnel disease. 5% of patients with heel pain has this triad. Recently Schon publishised that 23/38 patients studied with electromyography had signs of entrapment of tibialis posterior nerve.
What does the evidence say about what to inject?
Jain SK in FAI 2018 doesn’t find any difference between PRP and steroid injection, both being equally effective
Corticoid injections + local anesthetic has been the gold standard for years.
What is the Indication of this intervention?
Non allergic patients
Clinical diagnosis of plantar fasciitis
Treatment can be done by general doctors in the clinical setting of a general practice.
Only needed 1ml Corticosteroid (Trigon DePot, Celestone (bethametasone) or similar) and 1ml of Anesthetic (Mepivacaine 2% or bupivacaine 0,5%) and basic aseptic protocolos (gloves, sterile needle and local antiseptic)
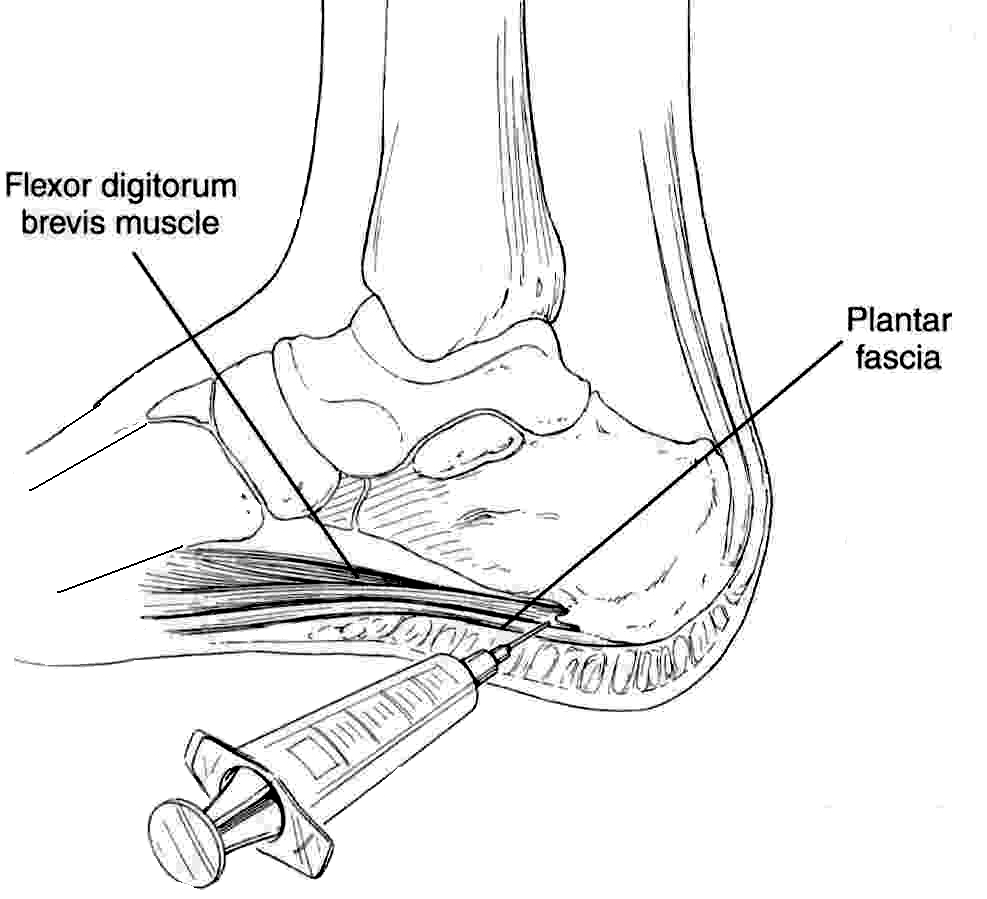
How to Inject local anesthetic in plantar fascia?
There are 2 main ways to inject the plantar fascia, firstly is to go perpendicular to plantar skin in the hot spot (major pain), another technique is to inject perpendicular to the plantar fascia from the medial side (Prefered method) where the skin is not so sensible and the injection is not so painful
Aspirate first and then inject above the plantar fascia in the proximal insertion.
How can we approach these patients systematically and based on evidence?
Routine medical history and anamnesis (activity level, BMI, job, alergies…)
Shoes? Previous treatments?
Exploration of the foot
Look for pain in the proximal medial side of plantar fascia
Pain with dorsiflexion
Hindfoot study (flatfoot or cavus foot)
Look for tight gastrocnemius - Silverskiold testing
Palpate tibial posterior tendon, achilles tendon and look for tarsal tunnel symptoms
If the diagnosis is clear:
Corticosteroid injection once on the plantar fascia (most painful point)
Teach about the diagnosis and explain the algorithm of treatment
Explain stretching and strengthening exercises.
AINE and acetaminophen
Lose weight
Stop sport and high activity until lessening of pain (Even stop weight-bearing for a few weeks)
Change of shoes, with wide comfortable soles, over the counter foot inserts and heel pads
Followup in a few months
If at 6 months there is no improvement with consservative treatment, look for other causes of heel pain and send to Rehab to do a shock wave therapy treatment
If at 9-12 months there is no improvement stil, send the patient to local orthopaedic surgeon to consider (proximal medial gastrocnemius recession or other surgical approaches)
Take Home Message
Plantar fasciitis can be clinically diagnosed
There needs to be a multilayered treatments answering many of the risk factors such as obesity, activity level and tight gastrocnemius
Corticosteroid injections remains as integral part of the treatment of this patients
Home Stretching programs and strengthening have been shown to be efective in a majority of patients (That are capable of keeping constant with the program)
Bibliography
Jain SK, Suprashant K, Kumar S, Yadav A, Kearns SR. Comparison of Plantar Fasciitis Injected With Platelet-Rich Plasma vs Corticosteroids. Foot Ankle Int. 2018 Jul;39(7):780-786. doi: 10.1177/1071100718762406. Epub 2018 Mar 30. PMID: 29600719.
Rathleff MS, Mølgaard CM, Fredberg U, Kaalund S, Andersen KB, Jensen TT, Aaskov S, Olesen JL. High-load strength training improves outcome in patients with plantar fasciitis: A randomized controlled trial with 12-month follow-up. Scand J Med Sci Sports. 2015 Jun;25(3):e292-300. doi: 10.1111/sms.12313. Epub 2014 Aug 21. PMID: 25145882.
Kamonseki DH, Gonçalves GA, Yi LC, Júnior IL. Effect of stretching with and without muscle strengthening exercises for the foot and hip in patients with plantar fasciitis: A randomized controlled single-blind clinical trial. Man Ther. 2016 Jun;23:76-82. doi: 10.1016/j.math.2015.10.006. Epub 2015 Oct 30. PMID: 26654252.
Siriphorn A, Eksakulkla S. Calf stretching and plantar fascia-specific stretching for plantar fasciitis: A systematic review and meta-analysis. J Bodyw Mov Ther. 2020 Oct;24(4):222-232. doi: 10.1016/j.jbmt.2020.06.013. Epub 2020 Jul 30. PMID: 33218515.
Johannsen FE, Herzog RB, Malmgaard-Clausen NM, Hoegberget-Kalisz M, Magnusson SP, Kjaer M. Corticosteroid injection is the best treatment in plantar fasciitis if combined with controlled training. Knee Surg Sports Traumatol Arthrosc. 2019 Jan;27(1):5-12. doi: 10.1007/s00167-018-5234-6. Epub 2018 Nov 15. PMID: 30443664.
Monteagudo M, Maceira E, Garcia-Virto V, Canosa R. Chronic plantar fasciitis: plantar fasciotomy versus gastrocnemius recession. Int Orthop. 2013 Sep;37(9):1845-50. doi: 10.1007/s00264-013-2022-2. PMID: 23959221; PMCID: PMC3764291. Link PDF
Maskill JD, Bohay DR, Anderson JG. Gastrocnemius recession to treat isolated foot pain. Foot Ankle Int. 2010 Jan;31(1):19-23. doi: 10.3113/FAI.2010.0019. PMID: 20067718.
Whittaker GA, Munteanu SE, Menz HB, Gerrard JM, Elzarka A, Landorf KB. Effectiveness of Foot Orthoses Versus Corticosteroid Injection for Plantar Heel Pain: The SOOTHE Randomized Clinical Trial. J Orthop Sports Phys Ther. 2019 Jul;49(7):491-500. doi: 10.2519/jospt.2019.8807. Epub 2019 May 26. PMID: 31130060.
Landorf KB, Menz HB. Plantar heel pain and fasciitis. BMJ Clin Evid. 2008 Feb 5;2008:1111. PMID: 19450330; PMCID: PMC2907928.
DiGiovanni BF, Nawoczenski DA, Lintal ME, Moore EA, Murray JC, Wilding GE, Baumhauer JF. Tissue-specific plantar fascia-stretching exercise enhances outcomes in patients with chronic heel pain. A prospective, randomized study. J Bone Joint Surg Am. 2003 Jul;85(7):1270-7. doi: 10.2106/00004623-200307000-00013. PMID: 12851352.
Kim C, Cashdollar MR, Mendicino RW, Catanzariti AR, Fuge L. Incidence of plantar fascia ruptures following corticosteroid injection. Foot Ankle Spec. 2010 Dec;3(6):335-7. doi: 10.1177/1938640010378530. Epub 2010 Sep 3. PMID: 20817847.
Samaila E, Colò G, Rava A, Negri S, Valentini R, Felli L, Magnan B. Effectiveness of corticosteroid injections in Civinini-Morton's Syndrome: A systematic review. Foot Ankle Surg. 2021 Jun;27(4):357-365. doi: 10.1016/j.fas.2020.05.001. Epub 2020 May 18. PMID: 32600970.